When a child says their tongue feels itchy or tingly after eating strawberries, it can immediately set off alarm bells for parents. Food reactions are especially worrying when they involve the mouth or throat, and it’s natural to fear something serious is happening. In many cases, however, this reaction is mild, short-lived, and not dangerous. Strawberries are a common fruit enjoyed by children, but they also contain proteins that can irritate sensitive mouths or trigger immune responses in some kids. Understanding the difference between a mild reaction and a true allergy helps parents respond calmly, avoid unnecessary panic, and still protect their child’s health and comfort.
The most frequent explanation for an itchy tongue after strawberries is a condition called Oral Allergy Syndrome, often shortened to OAS and also known as pollen–food allergy syndrome. This happens when the immune system confuses proteins in certain raw fruits with proteins found in pollens. If a child is sensitive to specific pollens, their immune system may mistakenly react when they eat a fruit with similar protein structures. In the case of strawberries, this confusion can cause quick, localized symptoms such as itching, tingling, or a mild burning sensation in the lips, tongue, roof of the mouth, or throat. These reactions usually begin within minutes of eating the fruit and tend to stay limited to the mouth rather than spreading through the body.
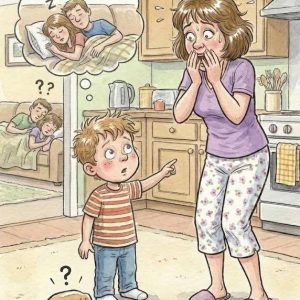
Parents should know what symptoms are typical and which ones signal something more serious. Common, mild signs include itching or tingling of the tongue or lips, slight swelling in the mouth, or a scratchy feeling in the throat that fades quickly once the child stops eating. These symptoms often disappear on their own within minutes. However, certain warning signs should never be ignored. Difficulty breathing, wheezing, a feeling that the throat is tightening, persistent or worsening swelling, vomiting, dizziness, or hives spreading across the body can indicate a more serious allergic reaction. If any of these occur, urgent medical care is necessary. Knowing these distinctions allows parents to act appropriately without overreacting to harmless symptoms.
Children tend to experience these reactions more often than adults because their immune systems are still developing and learning what is harmless and what is not. If a child already has seasonal allergies, especially during pollen-heavy months, their immune system may be on high alert. In this state, it is more likely to overreact to proteins in foods that resemble pollen proteins. This is why a child might eat strawberries without issue at one time of year but suddenly notice itching during spring or early summer. The reaction is not necessarily to the fruit itself, but to how the immune system is interpreting it at that moment.
This phenomenon is known as pollen–fruit cross-reactivity. The immune system recognizes certain fruit proteins as if they were pollen allergens, triggering a familiar allergic response. For example, children who react to birch pollen may also experience symptoms after eating apples, peaches, cherries, or strawberries. The body essentially mistakes the fruit for pollen and responds with itching or tingling in the mouth. Importantly, this does not usually mean the child has a dangerous food allergy. Instead, it reflects how closely related some plant proteins are and how sensitive the immune system can be when it is already primed by environmental allergens.
One helpful detail for parents is that raw strawberries are far more likely to cause symptoms than cooked or processed forms. Heat changes the structure of the proteins responsible for Oral Allergy Syndrome, making them less recognizable to the immune system. As a result, many children who react to fresh strawberries can still safely eat strawberry jam, sauces, yogurt with strawberry flavoring, or baked goods containing strawberries. Parents can manage mild symptoms by temporarily avoiding raw strawberries, keeping a simple food diary to track reactions, encouraging children to speak up immediately if their mouth feels itchy, and trying cooked alternatives instead. During heavy pollen seasons, reactions may be more noticeable, so extra caution can help. If symptoms are frequent, confusing, or extend beyond the mouth, seeing an allergist is a good step. An evaluation can confirm whether it is Oral Allergy Syndrome, rule out more serious allergies, and provide clear guidance. With awareness, simple substitutions, and careful monitoring, most children can continue to enjoy a varied and healthy diet without fear.